The best way to prevent stroke is to reduce your risk factors:
+ Treat and control high blood pressure and high cholesterol
+ If you smoke, stop smoking — many excellent smoking cessation programs are available; your health care provider can advise you about tools to use, such as the nicotine patch, as well as exercise and other changes in your activities.
+ Keep your weight within normal limits.
+ Exercise regularly; try for 5 days a week.
+ Eat a diet that is rich in fruits, green leafy vegetables, fish, whole grains, and nuts (especially walnuts).
+ If you have diabetes, keep it under good control.
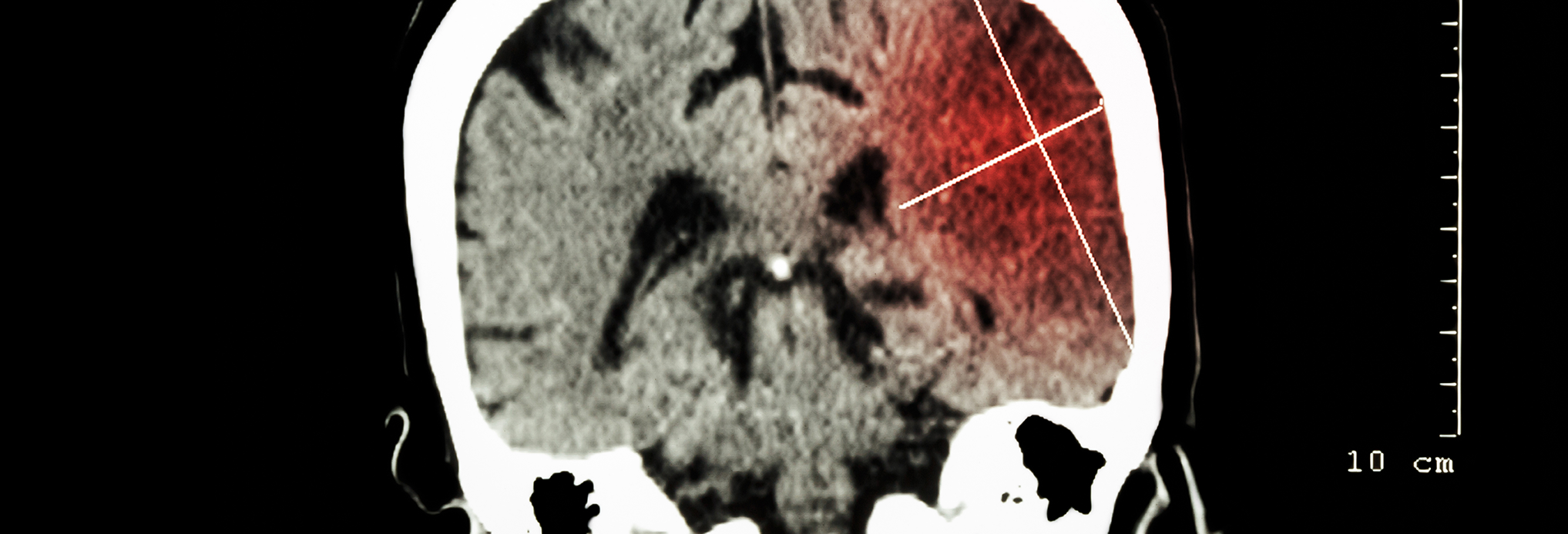
If you have heart disease or an abnormal heart rhythm, work with your doctor. Certain problems with the heart and blood vessels, such as atherosclerosis and atrial fibrillation, can cause blood clots to form. These clots can travel through the bloodstream and block an artery in the brain, causing a stroke (or can block a blood vessel in the heart and cause a heart attack).
Medications for prevention
+ Antiplatelet agents — These include aspirin and stronger prescription drugs like clopidogrel (Plavix). In one study, aspirin therapy reduced the risk of cardiovascular events, including stroke, by 21%. These drugs help keep tiny blood cells called “platelets” from clumping together in the bloodstream.
+ Anticoagulants — These drugs also prevent clots, but are much stronger than antiplatelet agents. Common anticoagulants are warfarin (Coumadin), Xeralto, Pradaxa and heparin (which is generally given at the hospital through injection into a vein).
Sub-links to the complete dietary supplement information
Nutrition and Dietary Supplements
Alpha-lipoic acid. Alpha-lipoic acid works together with other antioxidants, such as vitamins C and E. It is important for growth and helps to prevent cell damage.
Calcium – (what do you want to include here about benefits post-stroke?)
Folic Acid, Vitamin B6, Vitamin B12, and Betaine. Many clinical studies indicate that patients with elevated levels of the amino acid homocysteine are as much as 2.5 times more likely to suffer from a stroke than those with normal levels. Homocysteine levels are strongly influenced by dietary factors, particularly vitamin B9 (folic acid), vitamin B6, vitamin B12, and betaine. These substances help break down homocysteine in the body.
Some studies have even shown that healthy individuals who consume higher amounts of folic acid and vitamin B6 are less likely to develop atherosclerosis than those who consume lower amounts of these substances. One recent study found that lowering of homocysteine with folic acid and vitamins B6 and B12 reduced the overall risk of stroke, but not stroke severity or disability.
Magnesium. Population-based information suggests that people with low magnesium in their diet may be at greater risk for stroke. Some preliminary scientific evidence suggests that magnesium sulfate may be helpful in treating a stroke or transient ischemic attack. More research is needed to know for certain if use of this mineral following a stroke or TIA is helpful.
Omega-3 Fatty Acids. Strong evidence from population-based studies suggests that omega-3 fatty acid intake (primarily from fish) helps protect against stroke caused by plaque buildup and blood clots in the arteries that lead to the brain. In fact, eating at least 2 servings of fish per week can reduce the risk of stroke by as much as 50%. However, people who eat more than 3 grams of omega-3 fatty acids per day (equivalent to 3 servings of fish per day) may be at an increased risk for hemorrhagic stroke.
If you are pregnant, the U.S. Food and Drug Administration (FDA) recommends that you limit eating fish that have high levels of methyl mercury, such as tuna, shark, and swordfish. Methyl mercury has a potential risk to your fetus.
Vitamin C. Having low levels of vitamin C can cause damage to blood vessels and may lead to a stroke. Vitamin C supplements may also improve cognitive function if you have suffered from multiple strokes.
Vitamin E. Eating plenty of foods rich in vitamin E, along with other antioxidants like vitamin C, selenium, and carotenoids, reduces your risk for stroke. In addition, low levels of vitamin E in the blood may be associated with risk of dementia (memory impairment) following stroke. Animal studies also suggest that vitamin E supplements, possibly in combination with alpha-lipoic acid, may reduce the amount of brain damaged if taken prior to the actual stroke.
Coenzyme Q10 — Co Q10 works as an antioxidant and may reduce damage following a stroke. However, it may interfere with some blood-thinning medicines, such as warfarin (Coumadin) and others.
Selenium — Low levels of selenium can worsen plaque build up (atherosclerosis). However, it is not known if taking selenium supplements will help.
Herbs
The use of herbs is a time-honored approach to strengthening the body and treating disease. Herbs, however, contain active substances that can trigger side effects and interact with other herbs, supplements, or medications. For these reasons, you should take herbs only under the supervision of a health care provider knowledgeable in the field.
Garlic. Clinical studies suggest that fresh garlic and garlic supplements may prevent blood clots and destroy plaque. Blood clots and plaque block blood flow and contribute to the development of heart attack and stroke. Garlic may also be beneficial for reducing risk factors for heart disease and stroke like high blood pressure, high cholesterol, and diabetes. If you have diabetes, or take statins for high cholesterol, talk to your doctor before using garlic supplements.
Ginkgo (Ginkgo biloba). Gingko may reduce the likelihood of dementia following multiple strokes (often called multi-infarct dementia). It may help to prevent blood clot formation and may decrease the amount of brain damage following a stroke. More research in humans is needed. Ginkgo should not be used with the blood thinner warfarin (Coumadin) unless specifically instructed by your health care provider.
Turmeric (Curcuma longa). Turmeric may help reduce stroke and heart attack by lowering the bad cholesterol (LDL) that causes plaque build up. It can also prevent platelet build up along damaged blood vessels that can lead to blood clots. However, turmeric can cause your blood to thin, so if you are taking blood thinners like Coumadin, you need to consult your doctor.